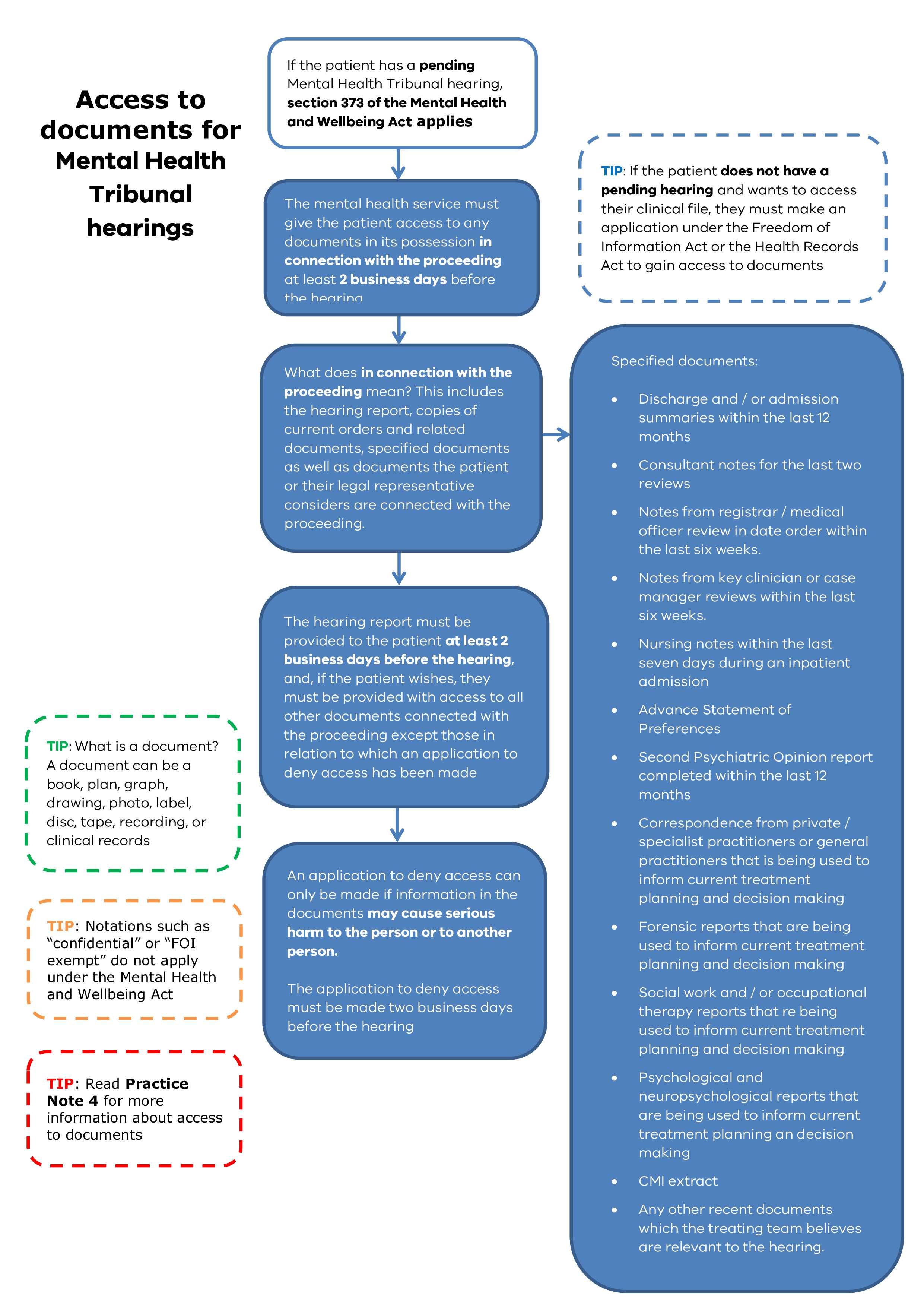
Overview of the requirement to provide access to documents
For fairness, the Mental Health and Wellbeing Act 2022 (MHW Act) requires the health service to give the patient access to documents ‘in connection with’ a Tribunal hearing at least 2 business days before the hearing.
An exception to this is that a psychiatrist may apply to the Tribunal to deny the patient access to a particular document or documents because disclosure of information in them may cause serious harm to the patient or another person.
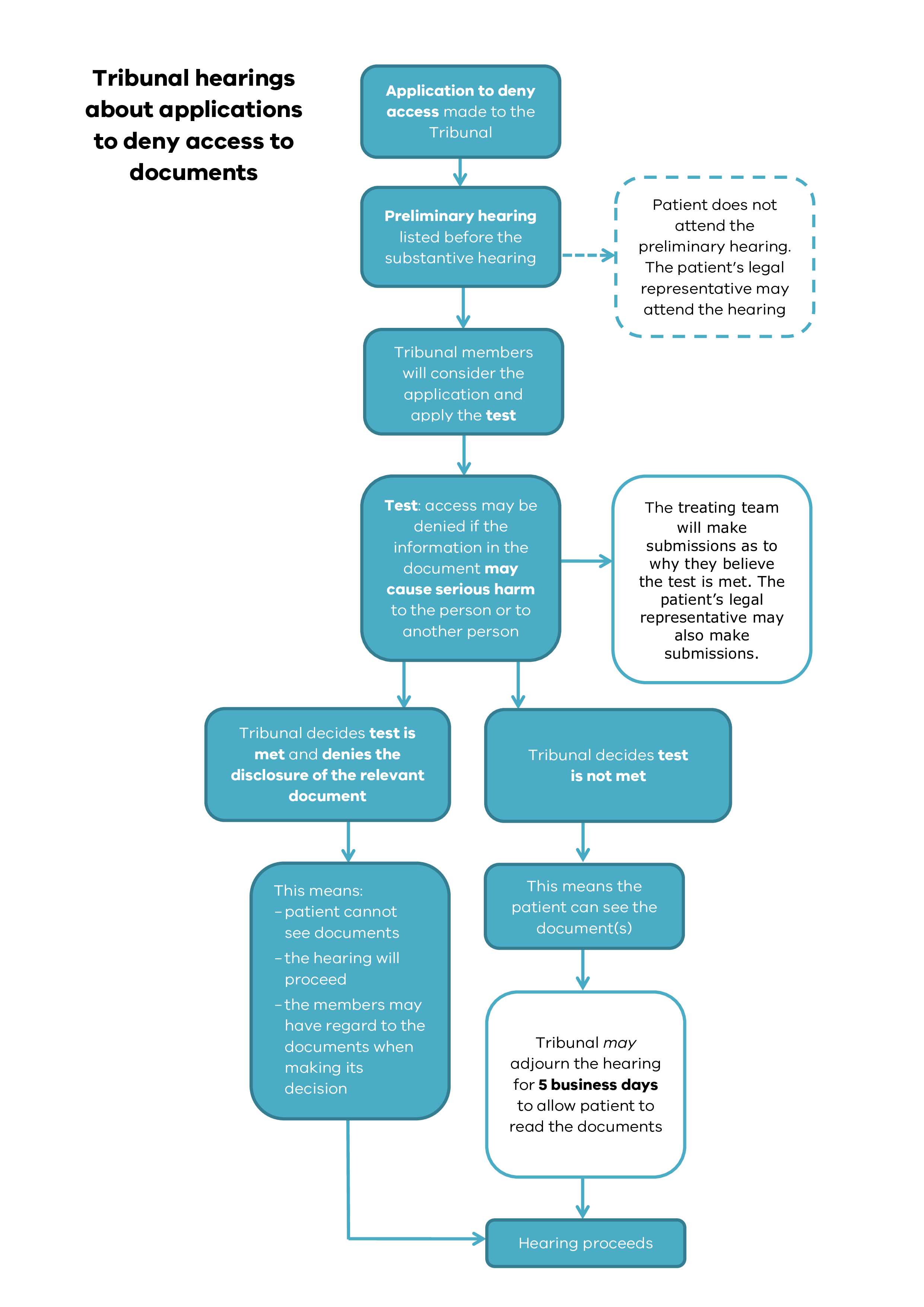
A psychiatrist can apply to the Tribunal to deny a patient access to documents by completing the Tribunal’s Application to deny access to documents (MHT 30) form.
When the Tribunal receives an application to deny access to documents (MHT 30) it will schedule a hearing for the application before the main hearing.
Patients are not allowed to attend hearings about applications to deny access to documents but are notified of the hearings so they can arrange for a legal representative to attend for them.
Documents that need to be provided – what documents are in connection with a proceeding?
The documents that are always connected with the proceeding are:
The relevant hearing report: This is the report that the Tribunal requires the health service to prepare before the hearing. The Tribunal has information and templates on its website to assist health services to prepare these reports.
Copies of current orders and related documents, specifically:
- Temporary treatment patient: the temporary treatment order, assessment order or court assessment order and any variations made by the authorised psychiatrist
- Treatment patient: the treatment order, any variations made by the authorised psychiatrist, and the Tribunal’s decision in any variation hearings and / or patient applications over the duration of the order
- Security patient: the secure treatment order or court secure treatment order, receipt of security patient form and Corrections Victoria Memorandum
- Forensic patient (ECT applications only): relevant order under the Crimes (Mental impairment and Unfitness to be Tried) Act 1997.
The following specified documents:
- Discharge and / or admission summaries within the last 12 months
- Consultant notes for the last two reviews
- Notes from the registrar / medical officer reviews in date order within the last six weeks
- Notes from Key Clinician or Case Manager reviews within the last six weeks
- Nursing notes within the last seven days during an inpatient admission
- Advance Statement of Preferences
- Second Psychiatric Opinion Report completed within the last 12 months
- Correspondence from private / specialist practitioners or general practitioners that is being used to inform current treatment planning and decision making
- Forensic reports that are being used to inform current treatment planning and decision making
- Social work and / or occupational therapy reports that are being used to inform current treatment planning and decision making
- Psychological and neuropsychological reports that are being used to inform current treatment planning and decision making
- CMI extract
- Any other recent documents which the treating team believes are relevant to the hearing.
Additional documents
In addition, the patient or their lawyer may place additional documents before the Tribunal provided that if the documents were not obtained from the mental health service they are also happy for the documents to be sent to the mental health service. See also the question below: ‘Can the patient or their lawyer request additional documents (not on the list of specified documents) from the mental health service or psychiatrist?’.
Applications to deny access to documents
A psychiatrist can apply to the Tribunal to deny a patient access to documents by completing the Tribunal’s Application to deny access to documents (MHT 30) form.
The completed form must be emailed to the Tribunal's Registry Team (registry@mht.vic.gov.au) at least 2 business days before the hearing date unless special circumstances apply (such as where the hearing concerned was listed as an urgent ECT hearing).
When the Tribunal receives an application to deny access to documents (MHT 30) it will schedule a hearing for the application before the main hearing.
Patients are not allowed to attend hearings about applications to deny access to documents but are notified of the hearings so they can arrange for a legal representative to attend for them.
Frequently asked questions
The right to access documents under the MHW Act only applies when there is a pending hearing. This means that the Tribunal registry has listed the hearing. A patient’s right to access documents under the MHW Act is separate from any rights they have under the FOI Act or the HR Act. This means a patient is not required to apply for access to documents connected with a pending hearing under the FOI or HR Act.
The MHW Act says that the health service must give the patient access to documents in connection with the proceeding at least 2 business days before the hearing. This means that the health service does not have to provide access any earlier than this (although it may do so).
The part of the MHW Act on access to documents only gives the patient the right to access documents. It does not say that nominated support persons or carers have any right to access documents. However, carers or nominated support persons may look at documents in connection with the hearing if the patient is happy for them to do so.
If there is no pending hearing, patients who wish to access their health information must apply to the health service under the FOI Act or the HR Act. The Tribunal is not involved in these processes.
The Tribunal has been advised that in some instances services require written authorisation from a patient before providing the patient’s lawyer access to documents that the patient is entitled to under section 373 of the Act. While this isn’t a matter specifically addressed by the Act, the Tribunal’s view is that if a lawyer provides written confirmation that they are representing a patient in their upcoming hearing, the ethical and regulatory framework covering such representations by a lawyer, mean that ordinarily separate, written authorisation from the patient is not needed. However, where a service has grounds for concern in a specific matter, obtaining separate authorisation may be appropriate.
In relation to documents that are the subject of an application to deny access, these documents can and should be given to a patient’s lawyer if the lawyer gives an undertaking not to disclose those documents or their contents to the patient. This will enable the lawyer to represent their client in the hearing of the application to deny access.
Yes. The Practice Note does not prevent the patient or their legal representative from requiring the designated mental health service or psychiatrist to provide additional documents that they (that is, the patient or their legal representative) consider are connected with the proceeding in any particular matter. Subject to any application to deny access to those documents, the designated mental health service or psychiatrist should provide these additional documents to the patient or their legal representative at least 2 business days before the hearing.
Where the patient or their legal representative request additional documents to those referred to in the Practice Note the designated mental health service or psychiatrist is not required to provide those documents to the Tribunal. The Tribunal expects the patient or their legal representative to provide the Tribunal with copies of the particular documents that they intend to rely on.
Yes, if the documents are:
- documents that will always be connected with the proceeding – i.e. the hearing report, the copies of current orders and related documents or a specified document, or
- additional documents the patient or their lawyer have requested from the mental health service or the psychiatrist that they believe are in connection with the hearing (see previous question).
A patient’s right to access documents under the MHW Act is separate from any rights they have under the FOI Act and HR Act. This means that notations in the clinical file that a document is ‘FOI exempt’ or similar do not mean that the patient cannot access these documents under the MHW Act.
The MHW Act requires the Tribunal to be satisfied that disclosing information contained in the document to the patient may cause serious harm. It does not have to be satisfied that disclosure would or would be likely to cause serious harm. In considering the serious harm test, the Tribunal will take into account the considerations in the list below. This list does not cover all of the things which the Tribunal may consider as this will depend on the circumstances of the case.
- ‘Serious harm’ may include a hurt, injury or damage that is important, demands consideration, is very considerable, or is significant (not slight, negligible or incidental)
- Potential harms that alone may not be sufficiently serious to demand consideration, might amount to serious harm when combined or taken together
- The Tribunal may also take into account:
- the psychological and physical health and wellbeing of the patient or another person (however, serious harm is not necessarily limited to physical or psychological injury).
- prejudice or damage to the patient’s prospects of successful treatment or recovery.
- prejudice or damage to relationships with persons who may support the patient’s recovery.
The patient’s psychiatrist can apply to the Tribunal to deny a patient access to documents by completing form MHT 30 Application to deny access to documents. This form can be downloaded from the Tribunal’s website at www.mht.vic.gov.au. The health service must return the completed form to the Tribunal’s registry via email to registry@mht.vic.gov.au at least 2 business days before the hearing date unless special circumstances apply (such as where the hearing concerned was listed as an urgent ECT hearing).
At the beginning of the hearing the Tribunal will generally ask the patient and the health service whether the patient has been able to access information in accordance with their rights under the MHW Act and the procedure in the practice note. The Tribunal expects the health service to give the patient the hearing report and help them to understand what it says. In addition, the Tribunal expects the health service to ask the patient whether they would like to access the other documents that it will provide to the Tribunal at or before the hearing.
If the health service has not given a patient access to documents in accordance with the MHW Act and the Tribunal’s practice note, the hearing may not be able to proceed. Whether it does or not will depend on whether the Tribunal considers that there can still be a fair hearing. An important consideration for the Tribunal will be the views of the patient, including whether they wish to read the documents that are connected with the proceeding. The Tribunal will also consider whether it was possible to provide access at least 2 days before the hearing and, if not, the reasons why it was not possible. Some examples where this may not be possible include when:
- the hearing involves an urgent application for ECT
- the patient or their lawyer has asked to see the documents to be provided to the Tribunal on the morning of the hearing (or otherwise less than 2 business days before the hearing) where the patient had earlier indicated that they did not wish to access them.
The Tribunal will consider the application to deny access to documents in a preliminary hearing that takes place before the hearing to discuss the main issues.
Preliminary hearing
The patient does not attend this preliminary hearing; however, their lawyer (if they have one) may do so. The Tribunal will also allow the lawyer to see any documents that the Tribunal views so long as the lawyer undertakes not to tell the patient what is in the documents.
At the preliminary hearing the Tribunal will ask the treating team to say why they believe the serious harm test is met.
Tribunal’s decision
After considering the issues, the Tribunal will either decide to grant the application (if it is satisfied that the serious harm test is met) or refuse the application (if it is not satisfied that the serious harm test is met).
If the Tribunal grants the application, this means that the patient cannot view or have a copy of the document(s).
If the Tribunal refuses the application, the Tribunal may order the health service to give the patient access to the document(s). It may also adjourn the hearing and extend the duration of the Order that the patient is currently on for up to five business days. This will give the patient time to access the documents(s) and prepare for the hearing. Alternatively, the Tribunal may decide to have a short break to allow the patient to view the document(s) before starting the hearing.
No. The health service cannot rely on a determination by a previous division of the Tribunal to apply in the future. A Tribunal decision under the MHW Act to grant an application to deny the disclosure of particular document(s) only applies to that particular hearing. If another hearing for the same patient is listed and the patient’s psychiatrist still believes that the serious harm test is met, they must apply to the Tribunal again.
No. The Tribunal does not have the power to consider a document without disclosing that document to the patient except when it receives an application to deny access to documents from the patient’s psychiatrist. Only the patient’s psychiatrist can ask the Tribunal to deny the patient access to a document or documents. This means the Tribunal cannot decide to deny access if it has not received an application from them.
For this reason, the Tribunal’s registry will not accept any document marked ‘confidential’, ‘private’ or ‘for the attention only of the Tribunal’ from carers, family members or other persons connected with a patient. The Tribunal’s registry will advise the sender of this and tell them to contact the patient’s treating team to discuss whether and how the documents can be provided to the Tribunal. The Tribunal’s registry will not forward such correspondence to the health service.
Similarly carers or family members cannot give the Tribunal documents that they wish to remain confidential on the day of the hearing.
The only grounds for deciding that a patient cannot have access to a certain document or documents connected with their hearing is that disclosure of the document(s) may cause serious harm to the patient or another person (i.e. the serious harm test). It may be that the Tribunal concludes that the serious harm test is satisfied in cases where a person provided information confidentially. However, this will not necessarily be the case. The Tribunal’s focus is on the serious harm test and not on whether the person providing the information wished it to be kept secret from the patient.
